‘Deaths of despair’ are rising. It’s time to define despair
By: Bruce Bower - Science News

Scientists investigate whether despair is distinct from mental disorders
Suicides are up...
but not in all demographics.
Low-education men.
Both White and Black.
Trump people...
Is there a link?

As 2015 wound down , a foreboding but catchy phrase from a scientific paper blew across the cultural landscape with unexpected force.

Researchers are developing ways to measure despair, distinct from any psychiatric ailment, that has contributed to deaths and mental suffering in the United States for several decades leading up to the current coronavirus pandemic.
JUANMONINO/ISTOCK/GETTY IMAGES PLUS
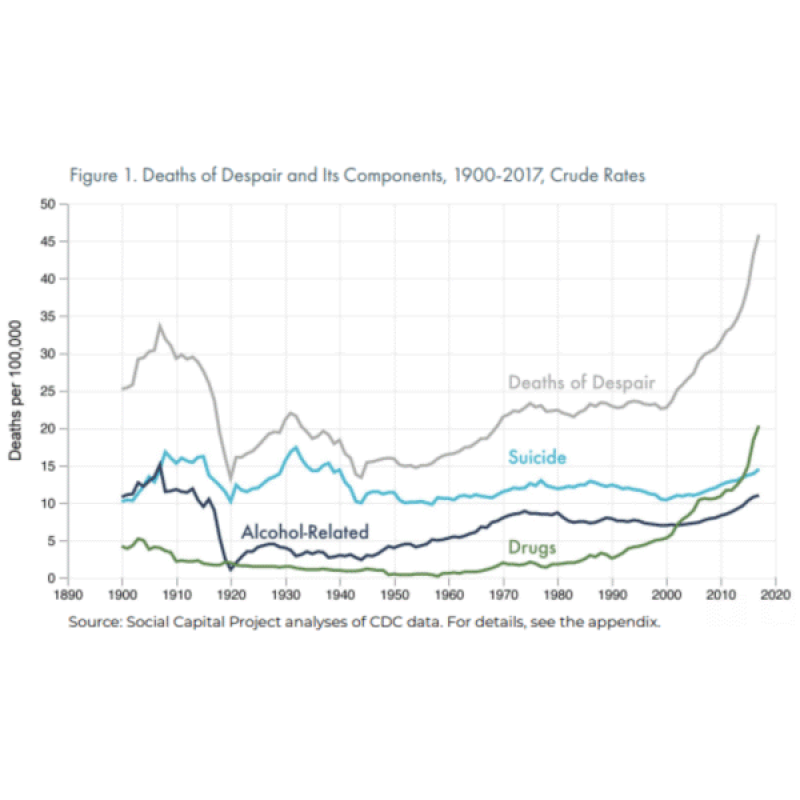
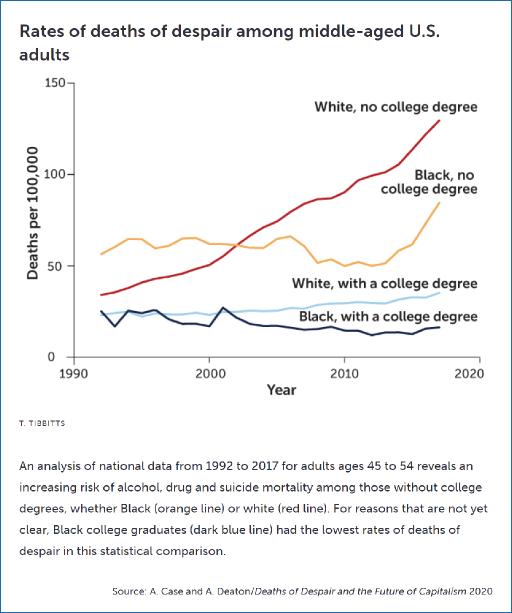
Since the 1990s, mortality had risen sharply among middle-aged, non-Hispanic white people, especially those without a college degree, Case and Deaton reported in December 2015 in the Proceedings of the National Academy of Sciences .
The reason, to a large extent: White, working-class people ages 45 to 54 were drinking themselves to death with alcohol, accidentally overdosing on opioids and other drugs, and killing themselves, often by shooting or hanging. Vanishing jobs, disintegrating families and other social stressors had unleashed a rising tide of fatal despair, Case and Deaton concluded. This disturbing trend mirrored what had previously occurred among inner-city Black people in the 1970s and 1980s, Case and Deaton now say. As low-skilled jobs vanished and families broke apart, Black victims of crack cocaine and the AIDS epidemic represented an early wave of deaths of despair. Even today, mortality rates for Black people still exceed those of white people in the United States for a variety of reasons, with Black overdose deaths on the rise over the last few years.
“The most meaningful dividing line [for being at risk of deaths of despair] is whether or not you have a four-year college degree,” Deaton says.
But despair has no clear scientific or medical definition. Psychiatric disorders plausibly related to a sense of despair, such as major depression and anxiety disorders, have been studied for decades. Despair — derived from a Latin term meaning “down from hope” — might be just another way to describe these conditions.
Or it might be its own special form of suffering. Some researchers regard despair as a distinct psychological status — one that can potentially be traced back to early childhood and may pose a risk for suicide, illegal drug use and maybe even physical pain.
For that reason, mental health clinicians need to work to distinguish despair from depression, even if despair isn’t a disorder in psychiatry’s diagnostic manual, says psychiatrist Ronald Pies of the State University of New York’s Upstate Medical University in Syracuse. “An overreliance on what is sometimes called ‘the Bible of psychiatry’ is likely to be misleading or inadequate when assessing the risk of suicide and illicit drug use,” he contends.
What’s more, recognizing and measuring despair, or something like it, as a state of mind separate from depressive disorders might shed light on the uptick in mental distress reported by people of all backgrounds during the coronavirus pandemic, Pies says. Developing a despair scale may also provide insights into those individuals most likely to succumb to despair-related fatalities. Long-term trends in national mortality data suggest that such deaths will continue to climb, even long after the viral calamity ends.
Downhearted minds
Case and Deaton’s emphasis on escalating 21st century deaths of despair — further detailed in their 2020 book Deaths of Despair and the Future of Capitalism — hit a nerve, especially among researchers studying groups of children as they grow into adults. These developmental scientists are in a prime position to uncover the roots of deadly despair and identify how some individuals nurture hope during difficult times while others experience a toxic brew of mental pain.
First, though, despair must be defined in a measurable way. In a study in the June JAMA Network Open , researchers described a preliminary assessment of a tool that can be used to estimate an individual’s level of despair . To develop the tool, psychologist William Copeland of the University of Vermont Larner College of Medicine in Burlington and colleagues focused on youngsters living in mostly rural parts of western North Carolina, a section of Appalachia that has been devastated by opioid overdoses and other deaths of despair. Known as the Great Smoky Mountains Study, the research was launched in 1992 and has assessed mental health in 1,266 individuals as many as 12 times, from ages 9 to 13 up to age 30.
Inspired by Case and Deaton’s findings, Copeland’s team looked at how despair has been defined in recent scientific studies and then reexamined the North Carolina data from a new perspective, identifying seven indicators of despair.
Two indicators — feeling hopeless and having low self-esteem — are among the symptoms of persistent depressive disorder, a psychiatric condition consisting of a depressed mood that lasts for at least two years in adults. Another indicator — feeling unloved — is a symptom of major depression, a mental disorder characterized by bouts of overwhelming sadness and social isolation lasting at least two weeks. A fourth indicator — worrying frequently — contributes to what mental health clinicians call generalized anxiety disorder. The remaining three indicators — loneliness, helplessness and feeling sorry for oneself — are not symptoms of any psychiatric disorder.
Combining those seven indicators into a despair scale let the researchers compare levels of despair among youngsters. Between 1 and 5 percent of children and teens in the study experienced at least one symptom on the scale in the three months before being interviewed, Copeland’s group reported. Among 25- to 30-year-olds, about 20 percent reported one despair item, and 7.6 percent cited at least two despair items, in the previous three months. Few participants suffered from more than five of the seven despair indicators. Individuals who cited single despair items related to depression rarely qualified for a depressive disorder in psychiatry’s diagnostic manual.
Young adults’ despair scores were generally higher among people who didn’t get a college degree and among African Americans in general.
Overall, 25- to 30-year-olds became increasingly likely to think about or attempt suicide and to abuse illicit drugs, including opioids, as they scored higher on the despair scale. These trends were especially strong among participants who had elevated despair scores that traced back to childhood.
In contrast to Case and Deaton’s national findings indicating that alcoholism contributes to deaths of despair, despair scores among participants displayed no link with alcohol abuse. Alcoholism is more widespread than suicide and opioid abuse, suggesting that excessive alcohol drinking stems from a wider range of stressful situations and personal problems than the other two behaviors do, Copeland says. As a result, any influence of despair on alcohol abuse may be difficult to pick up statistically.
And though lower education levels were associated with higher despair scores, Copeland’s team failed to find an elevated tendency of less-educated participants to become suicidal or abuse drugs. That finding deserves closer scrutiny in a nationally representative sample of young adults, not just rural North Carolinians, Deaton says. Further research also needs to expand the current despair scale to include other potential indicators of despair, such as sadness, recklessness and declining immune function, Copeland adds.
Despair as measured by the new scale represents a downhearted state of mind, not a mental disorder, Copeland suspects. High despair scores predicted illicit drug abuse and suicidal thoughts and behaviors regardless of whether 25- to 30-year-olds qualified as depressed. Despair was not usually accompanied by depression, though depressed participants typically reported experiencing indicators of despair, such as being lonely.
Scores on this instrument highlight growing concerns that a sense of despair contributes to self-destructive but not necessarily lethal behavior among people on the cusp of adulthood. “We’re seeing a large effect of despair on [some] young adults,” Copeland says. “It makes their lives miserable.”
There's a lot more, very much worth reading, in the OA . This has been sitting in my "to be seeded" file for a week... but the headlines have been kinda full...





Drugs are the proximate cause... but aren't drugs usually a symptom?
Modern people are inundated with information from all directions telling them overtly and subliminally that if they don't achieve material success they are losers. Such conclusions affect some more deeply than others.
The damage is worst among low-education males, where "success" is rare...