Is this the beginning of an mRNA vaccine revolution?
By: Adam Finn - The Guardian

No one knew whether mRNA technology would work - but it does.
It's an extraordinary moment for science, says academic Adam Finn
What is an "mRNA vaccine"?
I haven't the foggiest... but in these times,
my eye is drawn to the word "vaccine".
Let's look into it....

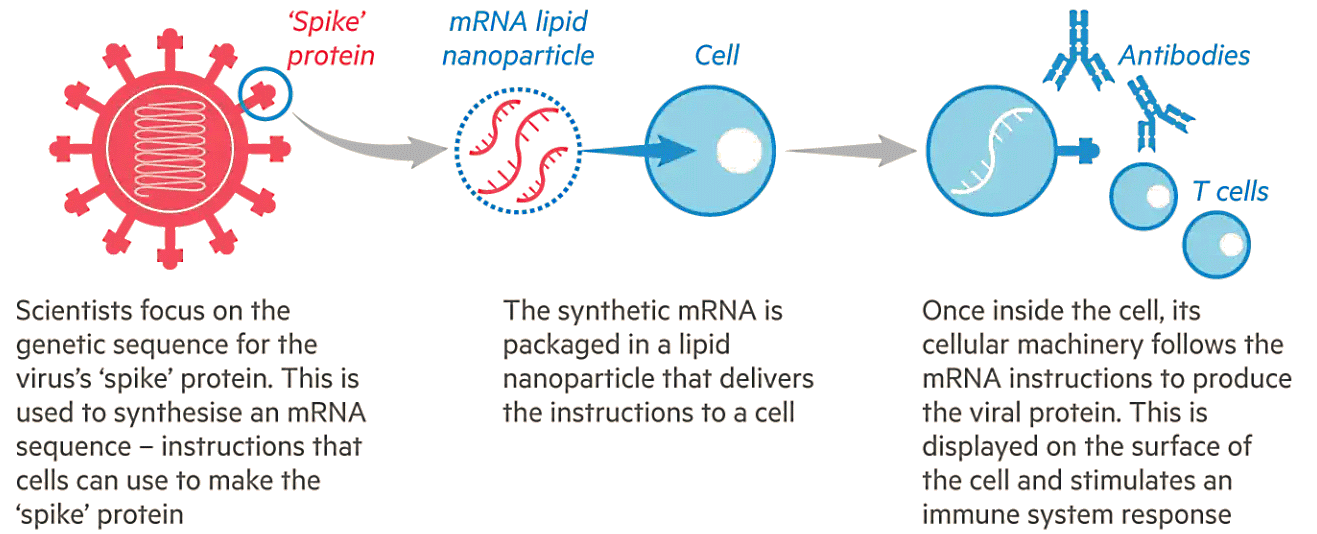
Essentially, mRNA is a molecule used by living cells to turn the gene sequences in DNA into the proteins that are the building blocks of all their fundamental structures. A segment of DNA gets copied ("transcribed") into a piece of mRNA, which in turn gets "read" by the cell's tools for synthesising proteins. In the case of an mRNA vaccine, the virus's mRNA is injected into the muscle, and our own cells then read it and synthesise the viral protein. The immune system reacts to these proteins - which can't by themselves cause disease - just as if they'd been carried in on the whole virus. This generates a protective response that, we hope, lasts for some time. It's so beautifully simple it almost seems like science fiction. But last week we learned that it was true.
It's extraordinary that observations originally made in cell cultures in a petri dish have been translated into real life. At the same time, it's not entirely surprising that the two first Covid-19 vaccines to announce phase 3 results were mRNA-based. They were first off the blocks because, as soon as the genetic code of Sars-CoV-2 was known (it was published by the Chinese in January 2020), companies that had been working on this technology were able to start producing the virus's mRNA. Making conventional vaccines takes much longer.
It's possible that the impressive performance of these new vaccines will eclipse that of the others currently in development. It depends on how effective those alternative approaches turn out to be - and results are going to start coming thick and fast. Beyond that, however, there's the question of whether mRNA could represent the future of all vaccines. If a coronavirus vaccine can be created this fast and this well with mRNA, why not use this approach across the board? In short: will mRNA become the default platform for vaccines from now on? That would mark a huge breakthrough in disease prevention.
We'll just have to wait and see if it happens. Even if we assume that the full detail of the results, when they come through, corroborates the headline figures, there are things that only time can reveal. How long will protection last, especially in those who are at greatest risk? Are these vaccines efficient enough not only to stop the recipients falling ill when exposed, but also to stop them getting infected altogether - or, failing that, to reduce the transmission of the virus to others?
The other key yardstick by which we judge any new vaccine technology is safety. Unlike drugs, which are given to treat people who are sick, vaccines are offered to everyone. Side-effects are only tolerable if they are pretty mild and short-lived - most people will accept a second of sharp pain followed by a tender upper arm and feeling a bit off-colour for a day or two, but that's all. Severe illness caused by vaccines should preferably be nonexistent, or at least vanishingly rare.
On the face of it, mRNA ought to be safe. After all, it is found in abundance in all the cells in our bodies all the time. It is also a very fragile molecule. It falls apart very easily and is rapidly broken down by proteins designed to do that, which seem to be everywhere. Working with mRNA in the lab is a nightmare because it keeps disappearing. On this basis, it should not hang around in the body for very long after it is injected.
The fact that mRNA is genetic material might lead you to think there's some risk of genetic side-effects. However, in human cells, while DNA is regularly transcribed into RNA, the reverse doesn't happen - RNA can't make it back into DNA and alter our genes. (In fact, making DNA from RNA - so called reverse transcription - is something that only a certain kind of virus, like HIV, can do). Ultimately though, confidence in the safety of vaccines is something that comes from experience, and it will be the same with mRNA. The reassuring thing is that they have been tested for safety in tens of thousands of study subjects already. Within a short time, that will become millions, and - assuming no unexpected problems appear - the sense of reassurance will grow.
Whether or not mRNA now becomes the preferred way to make novel vaccines, it is clear that a global disaster on the scale of the pandemic spurs innovation at a much faster rate. This is not just the consequence of all the resources and funding made available to those with solutions that might usually be regarded with more scepticism; it is also driven by the remarkable things that humans can achieve when thrust together by circumstances and given a common purpose. While we like to lionise individual heroes and leaders, scientific advances like mRNA vaccines are always the product of the collaborative efforts of many people with diverse skills and backgrounds. Bringing vaccines to the clinic also requires large numbers of brave and altruistic volunteers to take part in clinical trials.
Stepping back, one fact stands out. At the beginning of November, we still did not know whether or not any vaccine would be able to help us overcome this terrible disease. As the month draws to its close, we're certain that they can. However mRNA vaccines go down in the history books, that in itself is something to marvel at. Human ingenuity, invention and sheer hard work mean we are finally on the road out of this disaster.
Adam Finn is professor of paediatrics at the Bristol Children's Vaccine Centre, University of Bristol




Thank you, Professor Finn. I actually believe I understand.